Featured Articles

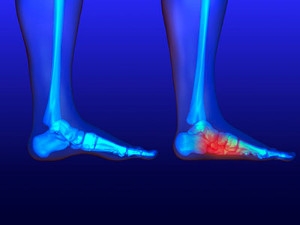
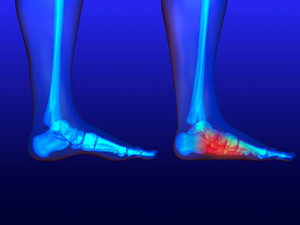
How Is Tarsal Tunnel Syndrome Treated?
 Tarsal tunnel syndrome is a condition in which the posterior tibial nerve, which runs through an area called the tarsal tunnel along the inside of the ankle, is compressed. This often occurs with other foot problems, such as plantar fasciitis or acquired flat foot. Tarsal tunnel syndrome causes sharp, shooting, electrical, dull, or burning pain sensations on the inner side of the ankle and in the heel. Treatment is almost always non-surgical and includes wearing comfortable shoes or orthotics, doing stretching exercises, modifying your daily activities to limit standing and walking while you heal, and taking nonsteroidal anti-inflammatory drugs to reduce pain. To learn more about treatment options for tarsal tunnel syndrome, please consult with a podiatrist.
Tarsal tunnel syndrome is a condition in which the posterior tibial nerve, which runs through an area called the tarsal tunnel along the inside of the ankle, is compressed. This often occurs with other foot problems, such as plantar fasciitis or acquired flat foot. Tarsal tunnel syndrome causes sharp, shooting, electrical, dull, or burning pain sensations on the inner side of the ankle and in the heel. Treatment is almost always non-surgical and includes wearing comfortable shoes or orthotics, doing stretching exercises, modifying your daily activities to limit standing and walking while you heal, and taking nonsteroidal anti-inflammatory drugs to reduce pain. To learn more about treatment options for tarsal tunnel syndrome, please consult with a podiatrist.
Tarsal tunnel syndrome can be very uncomfortable to live with. If you are experiencing tarsal tunnel syndrome, contact one of our doctors of Kitsap Foot & Ankle Clinic. Our doctors can provide the care you need to keep you pain-free and on your feet.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome, which can also be called tibial nerve dysfunction, is an uncommon condition of misfiring peripheral nerves in the foot. The tibial nerve is the peripheral nerve in the leg responsible for sensation and movement of the foot and calf muscles. In tarsal tunnel syndrome, the tibial nerve is damaged, causing problems with movement and feeling in the foot of the affected leg.
Common Cause of Tarsal Tunnel Syndrome
- Involves pressure or an injury, direct pressure on the tibial nerve for an extended period of time, sometimes caused by other body structures close by or near the knee.
- Diseases that damage nerves, including diabetes, may cause tarsal tunnel syndrome.
- At times, tarsal tunnel syndrome can appear without an obvious cause in some cases.
The Effects of Tarsal Tunnel Syndrome
- Different sensations, an afflicted person may experience pain, tingling, burning or other unusual sensations in the foot of the affected leg.
- The foot muscles, toes and ankle become weaker, and curling your toes or flexing your foot can become difficult.
- If condition worsens, infections and ulcers may develop on the foot that is experiencing the syndrome.
A physical exam of the leg can help identify the presence of tarsal tunnel syndrome. Medical tests, such as a nerve biopsy, are also used to diagnose the condition. Patients may receive physical therapy and prescriptive medication. In extreme cases, some may require surgery.
If you have any questions please feel free to contact one of our offices located in Bremerton and Port Orchard, WA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Treating Tarsal Tunnel Syndrome
Tarsal tunnel syndrome is a condition in which the tibial nerve, located in the tarsal tunnel in the foot, is compressed. The tibial nerve can become compressed from injury, such as an ankle sprain, flat feet, and lesions. Arthritis, diabetes, and varicose veins can also cause swelling and thus result in nerve compression.
Symptoms of tarsal tunnel syndrome include several different sensations in the sole of the foot, inside the ankle, and around the tibial nerve. These sensations include shooting pains, numbness or reduced sensation, pins and needles, burning, and tingling. Symptoms tend to worsen with greater activity to the area. In rare and severe occasions, this can change the muscles in the foot.
If you suspect you have tarsal tunnel syndrome, you should consult with your podiatrist. He or she will examine your medical history to see if you have a history of diabetes, arthritis, or flat feet. They will also check to see if you have suffered an injury to the area recently. An electrical test will be conducted to check if the nerve has been damaged. A simpler Tinel’s Test might also be used. This includes simply tapping the nerve to create a sensation. An MRI scan of the area may also be used.
Treatments vary greatly for tarsal tunnel syndrome. Treatments include both nonsurgical and surgical options depending upon the severity of the condition. Nonsurgical options include anti-inflammatory medication and steroid injections to the area. Orthotics, such as a splint or brace that immobilizes the foot, is another noninvasive option. For those with flat feet, custom shoes can be made to offer better foot support. Surgical options include a tunnel tarsal release, in which an incision is made behind the ankle down to the arch of the foot. This releases the ligament and relieves pressure off the nerve. Some doctors use a more minimally invasive surgery, where smaller incisions are made in the ankle and the ligament is stretched out.
If you are suffering from painful sensations in your foot, see a podiatrist who can determine if you are experiencing tarsal tunnel syndrome. Tarsal tunnel syndrome that is left unchecked can cause permanent nerve damage to the foot.
Why Does My Child Walk on Their Toes?
By monitoring a child’s foot development in the early years—and intervening if any structural abnormalities or dysfunction is present—the child’s quality of life can be vastly improved, and serious foot complications later in life may be avoided. Some milestones in a child’s early development are: sitting up by themselves at approximately 6-7 months, beginning to walk at roughly 12 months, and walking heel-to-toe by age 3 instead of on their toes as some toddlers do while learning to walk. Toe walking after age 3 may just be a habit, or due to a tight Achilles tendon, or it could possibly be an indicator of a muscular, neurological, or developmental issue the child may have. If you are concerned about your child’s foot development, schedule an appointment with a podiatrist for a full examination and consultation.
The health of a child’s feet is vital to their overall well-being. If you have any questions regarding foot health, contact one of our doctors of Kitsap Foot & Ankle Clinic. Our doctors can provide the care you need to keep you pain-free and on your feet.
Tips for Keeping Children's Feet Healthy
- Make sure their shoes fit properly
- Look for any signs of in-toeing or out-toeing
- Check to see if they have Clubfoot (condition that affects your child’s foot and ankle, twisting the heel and toes inward) which is one of the most common nonmajor birth defects.
- Lightly cover your baby’s feet (Tight covers may keep your baby from moving their feet freely, and could prevent normal development)
- Allow your toddler to go shoeless (Shoes can be restricting for a young child’s foot)
- Cut toenails straight across to avoid ingrown toenails
- Keep your child’s foot clean and dry
- Cover cuts and scrapes. Wash any scratches with soap and water and cover them with a bandage until they’ve healed.
If you have any questions, please feel free to contact one of our offices located in Bremerton and Port Orchard, WA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
How to Care for Your Child's Feet
It is never normal for a child to experience pain in his or her feet. Foot pain that lasts more than a few days and limits a child’s ability to walk should be examined by a podiatrist. Many adult foot ailments originate in childhood and may be present at birth. Common foot issues that are experienced by children are pediatric flat foot, Sever’s disease, ingrown toenails, and plantar warts.
A child’s foot grows rapidly during the first year, allowing it to reach almost half of their adult foot size. Consequently, foot specialists consider the first year to be the most crucial point in the foot development process. There are ways you can help ensure that your child’s foot develops properly. One way is to carefully look at your baby’s feet. If you notice any deformities, you should immediately seek professional care. You should also loosely cover your child’s foot, since tight coverings may prevent movement and inhibit normal development. Another tip is to change the baby’s positioning throughout the day. If your baby lies down in one spot for too long, it may put an excess amount of strain on the feet and legs.
It is best that you try not to force a child to start walking. Children will begin to walk when they are both physically and emotionally capable to do so. You should also avoid comparing your child’s walking progress with other children because the age range for independent walking may range. When your child’s feet begin to develop, you may need to change both their shoe and sock size every few months to allow room for their feet to grow.
Kids are sometimes prone to splinters, cuts, and severe injuries because they tend to walk around barefoot. This also makes them more susceptible to developing plantar warts which is a condition caused by a virus that invades the sole of the foot through breaks in the skin. These ailments can be avoided by making sure your child wears shoes in unsanitary environments. You should also wash any minor cuts or scrapes on your child’s feet. It is a myth that exposure to fresh air will heal injuries; fresh air will only expose your child’s cuts to germs.
As a parent, you should ensure that your child’s feet are developing properly and are being properly maintained. Consequently, it is important that you perform routine inspections on his or her feet to detect any injuries or deformities in their early stages. Early detection and treatment will help to ensure that your child does not develop any serious foot conditions.
Symptoms of Diabetic Neuropathy
 Diabetic neuropathy is a common complication of diabetes that causes nerve damage in the hands and feet. Neuropathy tends to develop slowly, sometimes over several decades, so people with diabetes are urged to closely monitor their foot health. The symptoms of diabetic neuropathy include a “pins and needles” sensation in the feet, sensitivity to touch or a loss of touch, pain, numbness, tingling, burning, difficulties with coordination while walking, and muscle weakness. Diabetic neuropathy can be dangerous and lead to serious complications, as the loss of sensation that it causes in the feet can make foot wounds more likely to form. These wounds tend to heal poorly and may become infected. If you have diabetes, a podiatrist can help you maintain the health of your feet.
Diabetic neuropathy is a common complication of diabetes that causes nerve damage in the hands and feet. Neuropathy tends to develop slowly, sometimes over several decades, so people with diabetes are urged to closely monitor their foot health. The symptoms of diabetic neuropathy include a “pins and needles” sensation in the feet, sensitivity to touch or a loss of touch, pain, numbness, tingling, burning, difficulties with coordination while walking, and muscle weakness. Diabetic neuropathy can be dangerous and lead to serious complications, as the loss of sensation that it causes in the feet can make foot wounds more likely to form. These wounds tend to heal poorly and may become infected. If you have diabetes, a podiatrist can help you maintain the health of your feet.
Neuropathy
Neuropathy can be a potentially serious condition, especially if it is left undiagnosed. If you have any concerns that you may be experiencing nerve loss in your feet, consult with one of our doctors from Kitsap Foot & Ankle Clinic. Our doctors will assess your condition and provide you with quality foot and ankle treatment for neuropathy.
What Is Neuropathy?
Neuropathy is a condition that leads to damage to the nerves in the body. Peripheral neuropathy, or neuropathy that affects your peripheral nervous system, usually occurs in the feet. Neuropathy can be triggered by a number of different causes. Such causes include diabetes, infections, cancers, disorders, and toxic substances.
Symptoms of Neuropathy Include:
- Numbness
- Sensation loss
- Prickling and tingling sensations
- Throbbing, freezing, burning pains
- Muscle weakness
Those with diabetes are at serious risk due to being unable to feel an ulcer on their feet. Diabetics usually also suffer from poor blood circulation. This can lead to the wound not healing, infections occurring, and the limb may have to be amputated.
Treatment
To treat neuropathy in the foot, podiatrists will first diagnose the cause of the neuropathy. Figuring out the underlying cause of the neuropathy will allow the podiatrist to prescribe the best treatment, whether it be caused by diabetes, toxic substance exposure, infection, etc. If the nerve has not died, then it’s possible that sensation may be able to return to the foot.
Pain medication may be issued for pain. Electrical nerve stimulation can be used to stimulate nerves. If the neuropathy is caused from pressure on the nerves, then surgery may be necessary.
If you have any questions, please feel free to contact one of our offices located in Bremerton and Port Orchard, WA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Neuropathy
Neuropathy is the weakness, numbness, and pain in the hands and feet due to damage to the peripheral nerves. The peripheral nerves are responsible for sending information from the brain and spinal cord to the rest of your body. Causes of Neuropathy include: traumatic injuries, infections, metabolic problems, exposure to toxins, and diabetes.
Diabetes is the most common cause, with more than half of the diabetic population developing some type of neuropathy. There are several types of neuropathy and they vary based on the damage of the nerves. Mononeuropathy is classified as only one nerve being damaged. When multiple nerves are affected, it is referred as polyneuropathy. One of the types of polyneuropathy is distal symmetric polyneuropathy. It is the most common for people with diabetes and starts when the nerves furthest away from the central nervous begin to malfunction. The symptoms begin with pain and numbness in the feet and then they travel up to the legs. A rarer form of polyneuropathy is acute symmetrical peripheral neuropathy, which is a severe type that affects nerves throughout the body and is highly associated with Guillain-Barre syndrome, an autoimmune disorder that attacks the peripheral nervous system and can be fatal. Although there are many types of neuropathy, most of them share the same symptoms such as pain, extreme sensitivity to touch, lack of coordination, muscle weakness, dizziness, and digestive problems. Since neuropathy affects the nerves, those affected should be careful of burns, infection and falling, as depleted sensations disguise such ailments.
The best way to prevent neuropathy is to manage any medical conditions such as diabetes, alcoholism, or rheumatoid arthritis. Creating and managing a healthy lifestyle can also go a long way. Having a healthy diet full of fruits, vegetables, whole grains and lean protein can keep the nerves healthy. These types of food have the nutrients to prevent neuropathy. Regularly exercising can help as well, but it is best to consult with a doctor about the right amount. In addition to diet and exercise, avoiding risk factors will also prevent neuropathy. This includes repetitive motions, cramped positions, exposure to toxic chemicals, smoking and overindulging on alcohol.
Why Does My Arch Go Away When I Stand?
While there are several different types of flatfoot, all of them involve a loss of the arch—either partial or total. Flexible flatfoot is a common form of this condition where the arch collapses upon standing and returns to normal when there is no weight on the foot. Because having flat feet changes the alignment of the foot (toes point outwardly, the heel points toward the outside of the foot, and the ankle turns in), people with this condition may be more prone to developing bunions and hammertoes. Flexible flatfoot may cause pain in various areas of the foot including the arch, heel, ankle, shin bone, or on the lateral side of the foot. Additionally, there may be some pain in the knee, hip, or lower back, and overall fatigue or aching in the feet or legs. A podiatrist can diagnose flatfoot through an examination and by taking an X-ray. Non-surgical treatment may involve shoe modifications, physical therapy, losing weight, modifying activities, or even wearing ankle or foot orthoses to help support your arches and adjust your gait. For a proper diagnosis and to determine what treatment option is best for you, it is suggested that you visit a podiatrist.
Flatfoot is a condition many people suffer from. If you have flat feet, contact one of our doctors from Kitsap Foot & Ankle Clinic. Our doctors will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact one of our offices located in Bremerton and Port Orchard, WA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Flat Feet
Flatfoot is a foot condition in which the arch of the foot has either partially or totally dropped or has never developed. While it is common in babies and small children, it can become a problem for them in adulthood if the arch never forms. For adults, the development of flat feet can be brought upon by injury, as a result of pregnancy due to increased elasticity, or obesity. Those who have health concerns such as rheumatoid arthritis or diabetes may also be at greater risk for developing the condition.
If you suspect that you have flat feet, it is best to consult your podiatrist. Your foot doctor will examine the suspected foot and observe how it looks while you sit and stand. He or she may take an X-ray to determine how serious the condition is. Some common signs of flatfoot include toe drift, in which the toes and front part of the foot point outward, a short Achilles tendon, and a heel that tilts outwardly while the ankle tilts inward.
Once flatfoot has been diagnosed, your podiatrist may suggest one of several treatment options. Flat feet can be rigid, in which the feet appear to have no arch even when the person is not standing; or flexible, in which the person appears to have an arch while not standing, but once standing the arch disappears. Those with flexible flatfoot may be told to reduce any activities that cause pain and to avoid extended periods of walking or standing. Another suggestion may be weight loss, as excessive weight may be placing pressure on the arches
In few cases, if the condition is severe and all other methods have been exhausted surgery may be required. This is normally avoided, however, due to a lengthy recovery time and high cost.
How Shoes Affect Your Plantar Fascia
The connective tissue on the bottom of your feet between your heel and toes is called the plantar fascia. That tissue can become aggravated from overuse, wearing high heels or shoes that change the shape of your foot when you walk, being obese, aging, having certain medical conditions, or being born with flat feet or high arches. This aggravation is called plantar fasciitis, and is the most common form of heel pain. Proper footwear may help avoid plantar fasciitis or reduce pain if it has already developed. Your shoes should allow the natural movement of your foot, and have cushioning that supports pressure points—especially the heel, while being flexible and offering proper arch support. A podiatrist can recommend shoes and even orthotics that can help your individual foot structure, while offering various treatments to relieve the pain and discomfort of plantar fasciitis.
It is important to find shoes that fit you properly in order to avoid a variety of different foot problems. For more information about treatment, contact one of our doctors from Kitsap Foot & Ankle Clinic. Our doctors will treat your foot and ankle needs.
Proper Shoe Fitting
Shoes have many different functions. They cushion our body weight, protect our feet, and allow us to safely play sports. You should always make sure that the shoes you wear fit you properly in order to avoid injuries and deformities such as: bunions, corns, calluses, hammertoes, plantar fasciitis, stress fractures, and more. It is important to note that although a certain pair of shoes might be a great fit for someone else, that doesn’t mean they will be a great fit for you. This is why you should always try on shoes before buying them to make sure they are worth the investment. Typically, shoes need to be replaced ever six months to one year of regular use.
Tips for Proper Shoe Fitting
- Select a shoe that is shaped like your foot
- Don’t buy shoes that fit too tight, expecting them to stretch to fit
- Make sure there is enough space (3/8” to ½”) for your longest toe at the end of each shoe when you are standing up
- Walk in the shoes to make sure they fit and feel right
- Don’t select shoes by the size marked inside the shoe, but by how the shoe fits your foot
The shoes you buy should always feel as good as they look. Shoes that fit properly will last longer, feel better, and improve your way of life each day.
If you have any questions, please feel free to contact one of our offices located in Bremerton and Port Orchard, WA . We offer the newest diagnostic and treatment technologies for all your foot care needs.